A Method for Assessing the Risks of Complications in Chemoradiation Treatment of Squamous Cell Carcinoma of the Head and Neck
Abstract
Background:
More than 500,000 new cases of squamous cell carcinoma of the head and neck (SCCHN) are registered annually in the world. 7,036 new cases of the disease were registered in Ukraine during 2018, about 35% of patients did not live even a year from the date of diagnosis as a modern standard for the treatment of patients with inoperable locally advanced SCCHN, chemoradiation treatment in the classical dose fractionation mode with chemo modification with cisplatin is used by specialists.
Objective:
The objective of this study is to analyze the effectiveness of chemoradiation treatment with cisplatin and 5-fluorouracil in the treatment of patients with SCCHN using modern mathematical models.
Methods:
During the investigation we assessed the effectiveness of treatment in 108 patients with locally advanced SCCHN (stages III, IVa, IVb). The results of calculating the probabilities of complications were obtained using the method of multivariate classification based on the radial basis ANN.
Results:
Analyzing the groups with different methods of chemo modification, we can conclude that the method of chrono-modulated radiochemotherapy with 5-fluorouracil and the chemoradiation therapy with cisplatin were almost equal in efficiency, namely 77% and 73.5%, respectively (p=0.35).
Conclusion:
Using the chemoradiation therapy with 5-fluorouracil in the treatment of patients with low somatic status and elderly patients is more expedient in contrast to the methods using cisplatin. The advantage of selection of mentioned treatment method is also confirmed by the results of calculating the average complication risks using the method of multivariate classification based on a radial-basis neural network.
1. INTRODUCTION
According to known data, more than 500,000 new cases of Squamous Cell Carcinoma of the Head and Neck (SCCHN) are registered annually in the world. 7,036 new cases of the disease were registered in Ukraine during 2018, about 35% of patients did not live even a year from the date of diagnosis. It should also be noted that among men aged 30-54 years, mortality from SCCHN ranks 5th among all oncopathology. Such data can be explained by the fact that 60% of patients with SCCHN in Ukraine begin treatment already at locally advanced stages of the disease [1, 2].
The selection of the treatment method depends on the location of the tumor, the patient's decision, and the available technical capabilities in the clinic. The existing variety of different methods for combined treatment dictates the need for constant efforts of specialists in an attempt to select the most rational treatment tactics.
A modern standard for the treatment of patients with inoperable locally advanced SCCHN, chemoradiation treatment in the classical dose fractionation mode with chemomodification with cisplatin is used by specialists. Such combination is significantly superior to the results of independent radiation treatment and polychemotherapy [3, 4]. To increase efficiency, researchers from all over the world are developing and testing new methods for fractionation of the radiation dose, which are new schemes of chemomodification and some of them are superior to the classical ones, which provides a basis for further research in mentioned direction [5, 6].
For assessing the treatment results, general statistical methods are used. However, having a large amount of input data, such as age, sex, disease stage, data from laboratory and instrumental testing, it is difficult to reliably estimate the benefits of one or another chemomodification method. In recent years, due to the development of information technology, using machine learning and artificial intelligence methods make it possible to conduct such an analysis.
In particular, to solve the problems of classifying and assessing the patient's condition or treatment results, the following methods can be used:
- Binary classification (decision trees and random forests) [7, 8];
- Artificial Neural Networks (ANNs) [9]: antireciprocal ANNs, radial basis ANNs, probabilistic ANNs;
- Multivariate logistic regression [10];
- Naive Bayesian classifier [11].
Each method has its advantages, disadvantages and application features [12, 13]. Since data on a patient's condition or treatment results can have a different nature, that is, be numerical, boolean or verbal, artificial neural networks were chosen to classify the patient's condition (or to determine the risks of complications) [14, 15]. These methods can process data of various types, and also allow not to involve experts or specialists in the field of statistics.
Considering the above mentioned, the main goal of our paper consists of analyzing the effectiveness of chemoradiation treatment with cisplatin and 5-fluorouracil in the treatment of patients with SCCHN using modern mathematical models.
2. MATERIALS AND METHODS
All investigations were carried out after obtaining informed consent from patients, taking into account the “World Medical Association Declaration of Helsinki. Ethical Principles for Medical Research Involving Human Subjects” [16] with all amendments and clarifications in 2008 under the supervision of the Bioethics Committee of IMRO NAMSU.
During investigation, we have assessed the effectiveness of treatment in 108 patients with locally advanced SCCHN (stages III, IVa, IVb) [17]. Patients’ treatment period is 2017-2018. Hospital - Grigoriev Institute for Medical Radiology and oncology of National Academy of Medical Sciences of Ukraine, Kharkiv, Ukraine. To achieve this goal, they were divided into 3 following groups:
- The 1st group (n=39), in which patients received treatment in a chronomodulated mode of hypofractionation of the radiation dose with chemomodification with 5-fluorouracil according to the developed technology;
- The 2nd group (n=34), where radiation therapy was used in the classical mode, which provides for fractionating the dose of 2 Gy to 60-70 Gy with chemomodification with cisplatin at a dose of 100 mg/m2 of body surface once every 3 weeks;
- The 3rd group (n=35) – the comparison group, in which the patients received independent radiation therapy in the mode of classical fractionating the dose of 2 Gy to 60-70 Gy.
The tested groups and the comparison group were presented considering age, stage and localization of the process.
The obtained data were generated in the form of a spreadsheet in Microsoft Excel 2016 and were subjected to statistical processing using the STATISTICA 12.0 program.
Quantitative indicators are presented in the form (X ± m), where X is the mean, and m is the standard error of the mean. For indicators characterizing qualitative characteristics, the absolute number and relative value in percent (%) were indicated.
The calculation of the indicators of one-year and two-year survival was carried out on the basis of survival curves according to the Kaplan-Meier method. Also, on their basis, the median survival rate was estimated as the time to death of half of the patients in the group.
The statistical significance of the differences was checked using a t-test for independent samples. Qualitative characteristics were compared using the log-rank likelihood test, Pearson's χ2. Differences were considered statistically significant at p <0.05.
The severity of early and late complications of healthy tissues, hematological toxicity was assessed in accordance with the Common Terminology Criteria for Adverse Events Scale (CTCAE v. 5.0, 2018 [18]). The degree of cancerous growth regression was assessed according to the RECIST v.1.1 [19] criteria.
3. MATHEMATICAL MODEL FOR ASSESSING THE RISKS OF COMPLICATIONS BASED ON AN APPLICATION
The results of calculating the probabilities of complications were obtained using the method of multivariate classification [20] based on the radial basis ANN.
Let us consider an algorithm for estimating the risks of complications based on a radial basis ANN with one hidden layer.
(1) A learning sample is used as input data for the ANN.
(2) Based on the results of ANN teaching, calculations are made for the check sample. The learning algorithm for radial basis ANN is described in [20].
(3) After completion of the ANN operation, the results of calculating the probabilities of complications are obtained.
As the input data (learning sample), the following data are used: test results, age and sex characteristics of the patient, etc. and the output data are estimates of the complication risks during treatment.
At the first stage, all input data must be normalized and made dimensionless. Normalization is necessary so that the values of all numeric input data belong to the same interval, for example {-3; 3}, and the output data belong to the interval {0; 1}.
Normalization is carried out using the following Eqn.:
where а and b are parameters which can be stated as a=3, b=3; x presents the current value of input sample; Xmax and Xmin correspond to maximum and minimum values of x
 .
.
To calculate the relative reduced error, the following Eqn. can be used:
where Δx presents absolute error of measuring.
For output data normalization the next Eqn. is used:

where parameter y denotes the estimate of complication and ymax presents its maximum value.
After normalization for the purpose of estimating the probability of possible complications, logistic transformation of data is carried out.
Since the range of possible probabilities can include zero, to solve the problem with division by zero, we use transformation to the new parameter z of logistic function using the Eqn.:

The inverse transformation
is used when a new patient appears and needs to choose a treatment program.
The results of treatment using various selected methods are presented as a function of the complication probabilities versus input data. Using a neural network model, the arguments of logistic functions corresponding to the input data are calculated. Based on the obtained arguments, the probabilities of complications and the average risks of complications are calculated. After comparison, the treatment method can be chosen, which corresponds to the lowest average risk.
To estimate the risks of complications when choosing a method for treating severe diseases that require an individual approach, the average Bayesian risk is used:

where
 represents the vector of complication risks of j type, and
represents the vector of complication risks of j type, and
 are jth type complication probabilities for ith treatment method.
are jth type complication probabilities for ith treatment method.
4. RESULTS AND DISCUSSION
Analyzing the response to the treatment in all groups of patients for whom a chemotherapy agent was added to radiation therapy, it can be concluded that the frequency of a positive response to treatment in them significantly was bigger than in other patients of comparison group. Analyzing the groups with different methods of chemomodification, we can conclude that the method of chronomodulated radiochemotherapy with 5-fluorouracil and the chemoradiation therapy with cisplatin were almost equal in efficiency, namely 77% and 73.5%, respectively (p=0.35).
Obviously, the survival rate plays the main role in the choice of a patient's treatment method. Therefore the analysis and comparison of these indicators have the greatest interest of scientists.
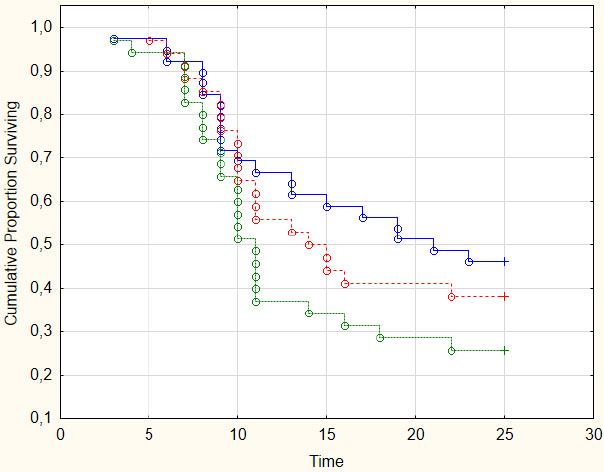
In our tests, the best survival rates were fixed in the 1st experimental group, for which 5-fluorouracil was used. Results are shown in Table 1.
| Type of Survival | Survival Percentage | |||
|---|---|---|---|---|
| Group 1 (n=39) | Group 2 (n=34) | Group 3 (n=35) | All groups | |
| One-year | 66.7±7.6 | 55.9±8.5 | 37.1±8.1 | 53.8±4.8 |
| Two-year | 46.2±8.0 | 38.2±8.3 | 25.7±7.4 | 37.0±4.6 |
The two-year survival rate when using chronomodulated radiochemotherapy with 5-fluorouracil (group 1) made value 46.2±8.0%, which is 1.2 times higher than the same indicator when radiation treatment using chemomodification with cisplatin (38.2±8.3%) (group 2), and 1.8 times higher than the indices of only radiation therapy (25.7±7.4%) (group 3). For a more accurate comparative analysis, survival curves were calculated using the Kaplan-Meier method and are demonstrated in Fig. (1). Results for group 1 are shown by blue solid line, for group 2 by red dashed line, and for group 3 by green solid line.
When comparing radiation toxicity with the use of various chemotherapy agents, it was observed that the development of grade 3 radiation mucositis in the 1st group was 5.3% less than in the 2nd group (p=0.32), but in the 2nd group, there were 2 cases (5.9%) of grade 4 mucositis, which required suspension of treatment, hospitalization and parenteral support of patients. The development of radiation dermatitis had the same level in all testing groups.
More significant differences were observed when analyzing the general reactions of patients to chemotherapy. Thus, the incidence of the general weakness of 2-3 degrees was 2.7 times higher in the group using cisplatin and amounted to 61.8%, in comparison with 23.1% in the group using 5-fluorouracil.
Dyspeptic symptoms were observed much more often in the 2nd group. So, nausea was observed in the 2nd group 11.5 times more often than in the 1st group and amounted 58.8% of cases in comparison 5.1% for the 1st group. Vomiting took place 9 times which made 23.5% of cases versus 2.6% for the 1st group. Correction of these disorders required the appointment of injectable antimimetics during the period from 3 to 7 days from the moment of the chemotherapy agent’s introduction. These unwanted events significantly disrupted the nutrition of patients. Therefore, in 26.5% of cases in patients of the 2nd group, a decrease in body weight by more than 10% was observed, and in patients of the 1st group by 12.8%, which was mainly a consequence of the development of radiation mucositis.
With regard to hematological toxicity, its occurrence depended to a greater extent on the chemotherapeutic agent, since in the comparison group, which received independent radiation therapy, only isolated disorders of 1-2 degrees were observed. There were no statistically significant differences in the development of anemia in both testing groups. So, in the 1st group, anemia was fixed in 18% of patients, and in the 2nd group in 23.5%, of which there was only one case of complications of grade 3. To correct anemia, only tablet forms of iron preparations were used. Blood transfusions and injectable preparations for correcting anemia were not used. Grade 1 leukopenia was observed in 20.5% of cases in the 1st group, while in the 2nd group, this indicator was 52.9%, which is a statistically significant difference (p=0.002). Patients with grade 1 leukopenia did not obtain additional medical correction and did not require a break in treatment. On the other hand, grade 2 leukopenia, requiring the introduction of colony-stimulating factors and steroid agents, and which was the reason for the delay in treatment for 2-5 days, was recorded in 5.1% in the 1st group and 11.8% in the 2d group (p=0.15). Grade 3 leukopenia was registered only in 2.9% of cases in patients of the 2nd group. In this group, thrombocytopenia of 1-2 tbsp was more often observed in 14.7% in comparison with 5.1% in the first group (p =0.08).
To comprehensively assess the effectiveness of the treatment method and its toxicity, we used a mathematical model, and as a result the following data were obtained.
The values of complication risks in the treatment by the three programs were calculated. Treatment programs were designated as follows: CRT1 - treatment in a chronomodulated mode of hypofractionation of the radiation dose with chemomodification with 5-fluorouracil, CRT2 - radiation therapy in the classical fractionation mode with chemomodification with cisplatin, RT - radiation therapy in the mode classic fractionation.
For each of the possible complications, the corresponding risk was assigned. The vector of complication risks is shown in Table 2.
| Type of Complication | Sign | Weight |
|---|---|---|
| Survival | С1 | 10 |
| Response of cancerous growth | С2 | 50 |
| Mucositis | С3 | 16 |
| Dermatitis | С4 | 7 |
| Leukopenia | С5 | 14 |
| Nausea | С6 | 3 |
The results of calculating the probabilities of complications for three treatment methods used to treat three control patients are presented in Table 3.
| Treatment Scheme | Patient | y10 | y20 | y30 | y40 | y50 | y60 |
|---|---|---|---|---|---|---|---|
| CRT1 | 1 | 0.01 | 0.25 | 0.75 | 0.49 | 0.25 | 0.49 |
| 2 | 0.01 | 0.55 | 0.66 | 0.01 | 0.01 | 0.01 | |
| 3 | 0.01 | 0.45 | 0.65 | 0.01 | 0.03 | 0.05 | |
| CRT2 | 1 | 0.57 | 0.56 | 0.86 | 0.55 | 0.01 | 0.01 |
| 2 | 0.68 | 0.75 | 0.75 | 0.25 | 0.49 | 0.01 | |
| 3 | 0.55 | 0.54 | 0.82 | 0.54 | 0.01 | 0.01 | |
| RТ | 1 | 1.00 | 1.00 | 1.00 | 1.00 | 0.24 | 0.24 |
| 2 | 1.00 | 1.00 | 1.00 | 1.00 | 0.23 | 0.23 | |
| 3 | 0.68 | 0.75 | 0.25 | 0.25 | 0.49 | 0.49 |
Average risks of complications calculated using the Bayes formula are given in Table 4.
| Treatment Scheme | Patient | ||
|---|---|---|---|
| 1 | 2 | 3 | |
| CRT1 | 33.00 | 38.35 | 33.84 |
| CRT2 | 51.40 | 64.94 | 49.5 |
| RT | 87.14 | 86.88 | 58.38 |
Having analyzed the obtained values of the complication risks for the methods of treatment for three patients, we can conclude that the first method of CRT1 has the least probability of complications. Thus, considered CRT1 method can be recommended for the treatment.
CONCLUSION
Analysis of the immediate and the nearest past results of the treatment by standard statistical methods, no significant differences in measures were found when using the developed method of chronomodulated radiochemotherapy compared to traditional chemoradiotherapy with cisplatin. At the same time, independent radiation therapy demonstrates significantly lower qualitative characteristics and, therefore can be recommended for patients with locally advanced forms of SCCHN only for palliative purposes. It should also be noted that cisplatin is highly toxic in combination with radiation therapy, in contrast to the chronomodulated introduction of 5-fluorouracil and so, using the chemoradiation therapy with 5-fluorouracil in the treatment of patients with low somatic status and elderly patients is more expedient in contrast to the methods using cisplatin. The advantage of a selection of mentioned treatment is also confirmed by the results of calculating the average complication risks using the method of multivariate classification based on a radial-basis neural network.
ETHICAL STATEMENT
All investigations were carried out taking into account the “World Medical Association Declaration of Helsinki. Ethical Principles for Medical Research Involving Human Subjects” [16] with all amendments and clarifications in 2008 under the supervision of the Bioethics Committee of IMRO NAMSU.
CONSENT FOR PUBLICATION
Informed consent was obtained from all the participant prior to data collection.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
FUNDING
This study was supported by National Academy of Medical Sciences of Ukraine (grant NAMS.04.12 “Comparative analysis of algorithms for opometric preparation and planning of conventional and conformal radiation therapy on a linear accelerator”, grant NAMS.02.17 “Development of personalized control of body, head and neck tumors during radiation therapy using in vivo dosimetry”).
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


