Three Waves of Substance-Induced Mental Disorders over the Past 30 Years: Results from a Retrospective Observational Cohort Analysis
Abstract
Introduction
Substance-induced disorders (SID) have gained increasing attention in recent years; however, there is insufficient data to fully understand the long-term dynamics of these conditions.
Materials and Methods
In a retrospective observational cohort study, we analyzed a publicly available database (Treatment Episode Data Set – Admissions) between 1992 and 2022 to determine cases of SID and to assess the influence of various independent clinical factors.
Results
Three waves in the dynamics of SID were identified. The first wave was from 1992 to 2001. The number of SID was minimal, with a predominance of men with an average age of 30-34 years, using mainly heroin, methamphetamine, or phencyclidine. The second wave was from 2002 to 2014. The total number of SID increased by 6.5 times, the percentage of women increased, the average age shifted to 25-29 years, and the predominant substances were opiates, stimulants, and barbiturates. The third wave, from 2015 to 2022, was characterized by continued growth in SID cases, surpassing the number of cases related to alcohol-induced disorders, substance abuse, and substance dependence. Methamphetamine and novel psychoactive substances play the most important role in the third wave.
Discussion
In some cases, SID can transform into a chronic relapsing psychiatric disorder, which will require creating special units for the dispensary monitoring to detect the transformation, as well as to provide comprehensive combined care.
Conclusion
SID is an actual problem. The number of these cases is growing faster than the general population of drug abusers, depending on the general drug situation.
1. INTRODUCTION
According to the World Health Organization's “Global Status Report on Alcohol and Health and Treatment of Substance Use Disorders” (2024), the impact of alcohol, tobacco, and substance use remains unacceptably high by any metric. Among individuals of working age, its health impact exceeds that of all other modifiable risk factors [1]. Substance use also has a significant impact on mental health, often increasing the severity of psychopathology, as well as contributing to high rates of premature mortality, including suicide [1]. According to the World Drug Report 2024, drug misuse has continued to increase in most countries of the world in recent years, mainly due to the demand for psychostimulants [2]. At the same time, the range of drugs has expanded, resulting in increasingly complex patterns of use, and polydrug use is common in most drug markets [2]. Countries in the Americas have one of the highest arrest rates for drug-related crimes [2].
Recently, the spectrum of mental disorders induced by substance use (SID) has attracted growing research attention. In ICD-11 and DSM-5, it is represented by a spectrum of mental health conditions: delirium, psychotic disorder, affective disorder, anxiety disorder, obsessive-compulsive disorder, and others [3]. There are often discussions about approaches to their diagnosis and prognosis [4, 5]. In recent years, a series of cases of induced psychiatric disorders after recreational drug use have been published [6]. However, there is a lack of data on the trends in the incidence of substance-induced mental disorders at a general population level. These data would allow a better understanding of the impact of the general addiction factors, including the emergence of novel psychoactive substances, on this type of addiction complication.
In the United States of America (USA), the Substance Abuse and Mental Health Services Administration website publishes publicly available files with complete datasets that are processed with full privacy protections [7]. They contain information on the demographic, clinical, and substance use characteristics of individuals who seek treatment in public or privately funded settings in the USA. In particular, the website contains the Treatment Episode Data Set on Admissions from 1992 to 2022, which collects all data from individuals at the time of treatment [7].
The objectives of this study were: 1) to analyze the absolute and the relative numbers of cases of SID in the period from 1992 to 2022, to classify them into sub-periods (waves) on the basis of clustering; 2) to compare the socio-demographic characteristics of persons with SID in different periods; 3) to investigate and compare the influence of different clinical factors on the incidence of SID in described subperiods.
2. MATERIALS AND METHODS
2.1. Study Design
The study has a retrospective observational cohort design with mixed (qualitative and quantitative) analysis.
2.2. Data Set
This study has analyzed the Treatment Episode Data Sets on Admissions (TEDS-A) data from 1992 to 2022. It is a publicly available de-identified dataset of drug treatment episodes. It collects socio-demographic data, diagnosis, and indications of preferred substances of abuse, frequency of use, and predominant mode of use. For the purposes of the research, the annual reports for the specified period were combined, with data being matched and harmonized for the purpose of the overall analysis. The total number of rows in the final dataset was 55,277,824, and the total number of columns was 41. Participant consent and ethical committee approval were not required for this research as the dataset is public and de-identified, and we are conducting only a secondary analysis.
2.3. Analyzed Sample
All cases with a diagnosis of Substance-induced disorder (code 2 in the ‘DSMCRIT’ column) were selected for analysis. As described in the Codebook of TEDS-A, these correspond to DSM diagnoses 292.00-292.99 or ICD-10 diagnoses F11.14-F11.99, F12.15-F12.99, F13.14-F13.99, F14.14-F14.99, F15.14-F15.99, F16.14-F16.99, F17.208-F17.299, F18.14-F18.99, and F19.14-F19.99. This sample did not include cases diagnosed with Substance abuse, Substance dependence, Alcohol-induced disorders, and primary psychiatric disorders (Anxiety disorders, Depressive disorders, Schizophrenic/other psychotic disorders, etc.) as they had a different code in this column. All rows with missing data were excluded from the analysis. A total of 543,697 cases of SID were selected using these criterias.
2.4. Analyzed Measures
2.4.1. Outcome Measure:
The primary outcome of research interest was the presence of SID among all treatment cases and the association of this diagnosis with the independent variables.
2.4.2. Independent Variables:
The independent variables were included:
- The year the patient was given treatment (a period of 30 years, from 1992 to 2022, was included);
- Patient-level variables:
- Patient age (11 age groups from ‘12-14 years’ to ‘55 years and over’ are represented in the database),
- Gender (male or female),
- Clinical characteristics:
- Type of treatment services or treatment setting (8 types)
- Type of most preferred illicit substance (alcohol was excluded from the analysis, leaving 17 groups of illicit substances)
- The type of substance use (‘Oral’, ‘Smoking’, ‘Inhalation’, ‘Injection’, ‘Other’),
- Frequency of substance use in the past month (there were three types - ‘No use in the past month’, ‘Some use’, ‘Daily use’)
- The count of treatment episodes prior to the current episode
- Age of first use of the most preferred substance
To compare the identified SID cases, the number of alcohol-induced disorders (AID), Substance dependence, and Substance abuse over the time period was also evaluated.
2.5. Data Analysis
The databases were analyzed using the R statistical package. Univariate statistics were used to characterize the full sample, as well as subsamples by gender and time periods. For clustering, we used the K-means method from the “ClusterR” package with determination of the optimal number of clusters using the “elbow” method and checking the quality of clustering using the “silhouette” method. The standardization of variables was not preceded before clustering because all variables were categorical, and special encoding was applied to convert them into binary variables before clustering. Correlation analyses were performed using Spearman's method. Comparison of the obtained clusters by individual categorical variables was performed using the chi-square method with Bonferroni correction for multiple comparisons. A binary logistic regression model (family ‘binomial’) was used to examine the odds ratio of the presence of SID as a function of independent clinical variables. When we built the models, rows with undefined values (-9) were removed, and the samples were balanced by the ‘undersample’ method. We split our dataset randomly into training (80% of the data) and test (20% of the data) sub-sets, which were balanced. The models built on the training sub-set were further validated on independent test sub-data, which confirms the validity of these models. The statistical significance of differences between logistic regression coefficients at different time intervals was determined using the Wald method. The GGStats package (v. 0.8.0) was used for plotting. Results from the logistic regression models were presented as the logarithm of odds ratios (log(OR)). Statistical significance was set at p < 0.05.
3. RESULTS
3.1. Analysing the Trends in the Prevalence of SID Cases Over the Period 1992-2022
Fig. (1) shows the trend in the proportion of SID cases among all the dataset cases over the full studied period. For comparison, this plot also shows the trend in cases of alcohol-induced disorders (AID) over the same period. Overall, the number of SID cases increased almost 49 times in absolute count (maximal 48,797 cases in 2018 vs. minimal 1,000 cases in 1993) or 24.7 times in relative terms (from 0.1% in 1992 to 2.8% in 2021). Moreover, the increase in SID did not correlate with the total number of cases per year (rS = 0.296, p = 0.1), confirming a true increase in SID cases. Cases of other substance use disorders increased during the study period, and their dynamics are positively significantly correlated with the dynamics of SID: AID (rS = 0.864, p < 0. 001), substance dependence (rS = 0.985, p < 0.001), substance abuse (rS = 0.873, p < 0.001), but the growth of the mentioned diagnosis during the studied period was only in 12.4, 8 and 4.8 times in absolute terms, respectively Table S1. Thus, between 1992 and 2022, there was a 49-fold increase in SID referrals, and this increase is several times greater than the overall increase in all other substance use disorders.
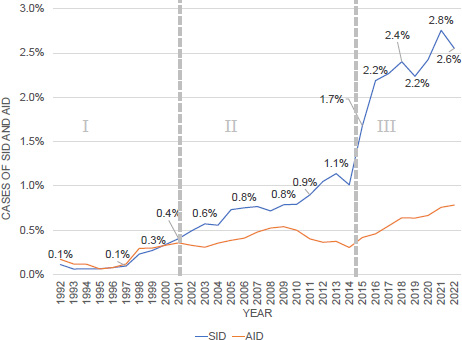
The percentage of patients with substance (SID) and alcohol (AID) induced disorders from the total number of patients per year (the x-axis represents the years included in the analysis, the y-axis represents the number of SID (blue line) and AID (orange line) patient visits; roman numerals I, II and III show the waves resulting from clustering).
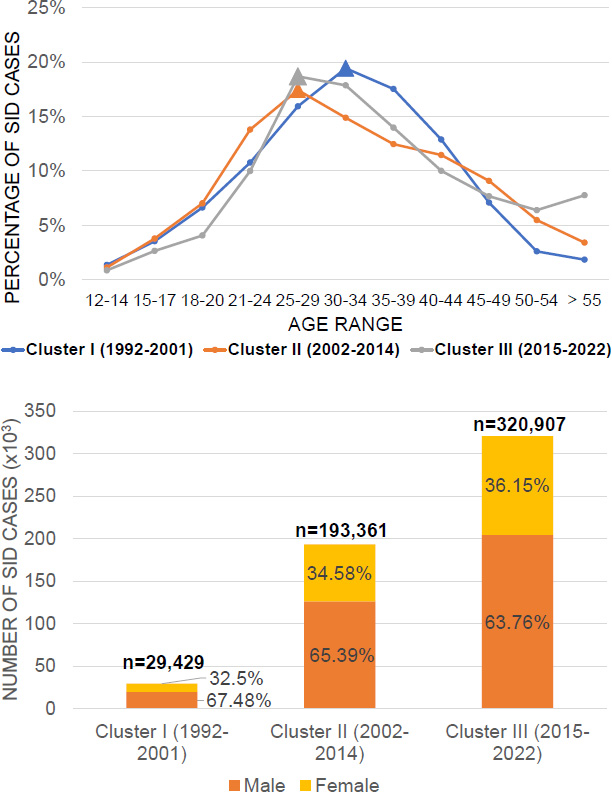
Comparison of clusters by gender-age characteristics (p<0,001 for all comparisons) (Graph A shows the percentage of patients with SID (vertical axis) by age (age ranges are presented on the horizontal axis. Graph B shows a diagram comparing the gender structure of patients with SID in the three analyzed periods).
After calculating the annual totals for the gender and age composition of SID patients, the resulting data array was subjected to cluster analysis. The optimal number of clusters was calculated as k=3 by the “elbow” method (Fig. S1). Further clustering was carried out by the k-means method, and 3 clusters were identified, which unite three time periods: Period I - from 1992 to 2001, Period II - from 2002 to 2014, and Period III - from 2015 to 2022 (Fig. S2). These periods represent three conditional waves of SID, and each of the waves had different socio-demographic and clinical characteristics. The quality of clustering using the silhouette methodology is 0.6885, which corresponds to good quality (Fig. S3). The other data will be further analyzed within the three selected time periods.
3.2. Analysis of Social and Demographic Characteristics of SID Cases
The frequency distribution of cases of SID referrals by gender and age characteristics is summarized in Fig. (2). In addition to the increase in the total number of cases in each cluster compared to the previous cluster, the proportion of female patients among SID cases also increased (from 32.5% in cluster I to 36.15% in cluster III). Also, in clusters II and III, the maximum number of referrals was recorded among persons of a younger age than earlier (25-29 years vs. 30-35 years), with a significant increase in the number of persons over 50 years in cluster III compared to the other two clusters. Thus, the first wave can be characterized as a wave involving predominantly men aged 30-35, while the second and third waves can be characterized as waves where the proportion of women consistently increases and where there are two age peaks: 25-35 years old and over 50 years old (Table S2).
When we assess the other characteristics of the patients, it is noteworthy that in the third cluster, the number of cells with missing values increased significantly (33.5% for educational level and 21% for marital status), which may reflect the dropout of these parameters for statistical analysis due to the nature of the data collection process (Table S3). Overall, all three clusters were characterized by a predominance of patients who had completed grade 12 (39.3% for cluster I, 42.5% for cluster II, and 33% for cluster III) and had never married (48.6% for cluster I, 58.4% for cluster II and 56.4% for cluster III).
3.3. Analysing the Effect of Clinical Characteristics on SID Detection
Fig. (3) shows the results of analysing the impact of clinical factors on SID in the three clusters under consideration Table S4.
When the logistic regression models were constructed for the variables 8 - Ambulatory, detoxification (in “Services”), 0 - No prior treated episodes (in “Previous treatment episodes”), 5 - Other (in “Route of administration”), 3 - Daily (in “Frequency of use”), were excluded from the analysis because coefficients could not be calculated. These variables had a very low presence in the dataset, so they did not play a significant role in the models.
All three models showed statistically significant differences from one another (p = 0.01), indicating that the three identified waves were characterized by distinct influences of clinical parameters, which were likely shaped by the evolving drug landscape Table S5. During the first wave, SID patients most commonly sought short-term 24-hour detoxification or brief inpatient rehabilitation, with minimal need for other forms of care. This trend persisted in the second and third waves, where there was a statistically significant pattern of low demand for additional treatment modalities.
The waves differed significantly in the number of previous treatment visits that preceded this episode: for the first cluster, among patients with SID, those who had 4 or 5 previous treatment visits were prevalent; for the second cluster, the number of previous visits had little impact on the chances of detecting SID; and for the third cluster, all values of the number of previous visits (from 1 to 5) had a negative coefficient. It can be assumed that patients with SID from the third wave had the first treatment.
Among the effects of route of drug administration on the detection of SID, all three clusters were characterized by a negative effect of oral use, with injecting having a positive effect in the first cluster and smoking having a positive effect in the third cluster. The influence of the route of administration was indirectly related to the most preferred substance. Regarding previous treatment episodes among individuals with substance use disorders, the category 'Some use' showed a small but statistically significant positive association in the third wave. In contrast, this parameter had negative coefficient values in the first and second clusters.
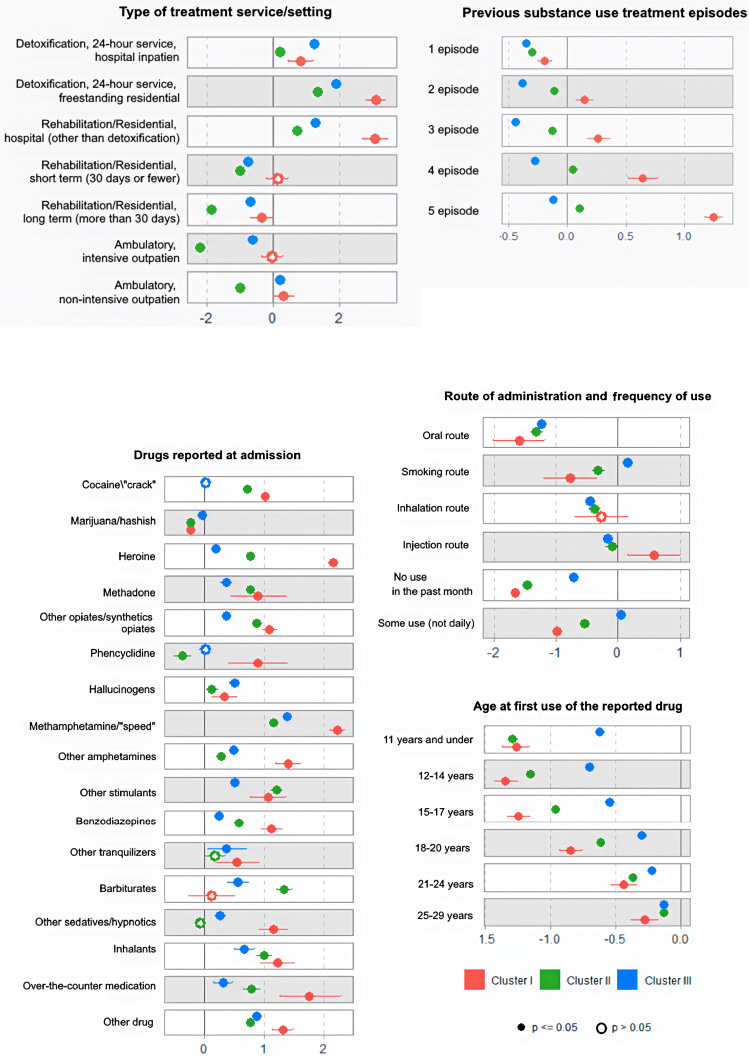
Log (OR) for logistic regression models with comparison coefficients among three clusters (red color shows the impact of factors on the 1st wave, green - on the second wave, blue - on the third wave).
The effect of age of onset showed a statistically significant negative association across all age variables. However, the magnitude of the coefficients decreased across clusters: the second cluster had smaller absolute values than the first, and the third had smaller absolute values than the second. This suggests a diminishing negative influence of onset age over time. If this trend continues, the age of onset may eventually show a positive association with the likelihood of detecting substance-induced disorders.
When assessing the impact of the preferred drug type on the likelihood of detecting SID, it is noteworthy that all drug classes, with the exception of marijuana, exhibited a statistically significant positive association with SID detection. The first wave was predominantly characterized by the use of heroin and methamphetamine, and uniquely showed a positive association with phencyclidine, a trend not observed in the other clusters. The second wave was predominantly ‘opiates/stimulants/barbiturates’, and the final third wave was predominantly ‘methamphetamine’ and the ‘Other drug’ group, in which novel psychoactive substances were counted.
4. DISCUSSION
When considering the impact of substance use on mental health, research has traditionally focused on harmful use, dependence, and withdrawal syndromes. However, in recent years, there has been a notable increase in the number of individuals seeking treatment primarily for substance-induced mental disorders. In updating the international classifications for this group of disorders, more diagnostic options have been formulated, which also reflects the increasing relevance of this group of disorders. Studies have been conducted that estimate the prevalence of selected types of induced mental disorders. National cohorts in Scandinavian countries have estimated the number of substance-induced psychoses and the risk of their transformation into schizophrenia and bipolar affective disorder [8-10]. In a meta-analysis by Murrie et al., it was reported that, on average, about 25% of substance-induced psychoses develop into schizophrenia, with the highest risk of transformation in psychoses associated with cannabinoids, hallucinogens and amphetamines and the lowest risk associated with opioids, alcohol, and sedatives [11].
In the USA, the National Epidemiological Survey on Alcohol and Related Conditions estimated the incidence of mood disorders induced by all classes of drugs as 0.26% [12], and among patients with psychostimulant dependence syndrome, the incidence may be as high as 64% [13]. For cocaine users, a study conducted in Spain found that substance-induced depression occurred in 61.3% of cases. Also, some clinical and biological markers for cocaine-induced depressive disorders were developed [14]. There is also research on the increased risk of induced OCD in drug users [15]. The data we have obtained on all SIDs complement the existing research and provide a comprehensive assessment of the scale and dynamics of these conditions over the past 30 years. The identification of three waves by cluster analysis shows that this process has its own internal regularities, which are related to the influence of sociodemographic and clinical variables.
Positive correlations were observed between the growth of SID, alcohol-induced disorders, substance dependence, and substance abuse, indicating that these conditions are influenced by the broader context of drug use trends. In our opinion, this may be due to the increasing use of synthetic novel psychoactive substances, which are more highly biochemically potent than their natural analogues. The first and second waves of SID were more associated with injecting heroin and smoking methamphetamine, while the third wave was associated with novel synthetic substances. The third wave started in 2014, and we have seen an increase in the annual detection of new substances, which are significantly higher than their natural equivalents in terms of the number and severity of complications [16]. We also found an increase in the number of women in the third wave compared to the first wave, which corresponds to the description of trends toward the erasure of gender differences and equalization of the share of men and women among drug users in recent years [1]. Additionally, the rise in the proportion of patients over 50 years old during the third wave aligns with general trends, indicating a growing prevalence of substance use among older age groups [2].
All patients with SID, irrespective of the period, favored short-term care in the form of 24-hour detoxification and continuation of treatment in the form of short inpatient rehabilitation. This coincides with the general conceptualization of SID as conditions arising from substance use and lasting up to 2 weeks. However, in some cases, SID can transform into a chronic relapsing psychiatric disorder, which will require a different type of care. The establishment of specialized units for follow-up clinical monitoring of patients with SID remains an important topic for further discussion, particularly to identify diagnostic transitions and to deliver comprehensive, integrated care. It is especially relevant for patients with substance-induced psychosis.
We have found a new approach to studying SID at the population level, demonstrated its relevance, and built the first population-based predictive models to identify these patients among all those who come for treatment. In the future, our approach and our results can be used to build medical decision support systems, digital screening applications, and personalized prevention programs.
5. LIMITATIONS
Limitations of this paper include the inability to categorize SID cases into separate disorders (delirium, psychosis, affective disorder, etc.). This limitation stems from the data collection methodology of the dataset used and may be addressed in future studies. Additionally, this dataset is subject to potential distortion of statistical relationships due to repeated admission bias, as it does not allow for the identification of unique patients since only referral cases are recorded [17]. This limitation does not significantly affect our results due to the chosen study design. The use of other methods and approaches for clustering is a perspective for further research. Also, in the future, more accurate statistics on individual cases of patients with SID can be provided through prospective clinical studies. The new DSM classification approaches help to better identify this group of cases.
CONCLUSION
Our findings highlight the importance of SID for public health, as the number of SID cases is increasing, and this trend is driven by many clinical and social factors. Probably, this group of patients will require specialized approaches to therapy and monitoring. Studying the results of SID cases in other countries will help to understand the influence of geographic and cultural factors on these disorders. In the future, special clinical monitoring and prevention protocols should be developed for patients with SID, as they can be viewed as an ultra-high-risk group for the development of chronic mental disorders. Due to the persistent development of increasingly highly potent designer drugs and the increase in the proportion of patients with combined use of several drugs, an increase in SID can be expected in the coming years.
AUTHORS’ CONTRIBUTIONS
The author confirms sole responsibility for the following: study conception and design, data collection, analysis and interpretation of results, and manuscript preparation.
LIST OF ABBREVIATIONS
| SID | = Substance-induced disorders |
| AID | = Alcohol-induced disorders |
| TEDS-A | = Treatment Episode Data Sets on Admissions |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Ethical approval was not necessary because the article used the publicly available de-identified dataset and performed only secondary analysis.
CONSENT FOR PUBLICATION
Participant consent was not required for this research as the dataset is public and de-identified.
AVAILABILITY OF DATA AND MATERIALS
The data that support the findings of this study are available in Treatment Episode Data Sets (TEDS) in the public domain: https://www.samhsa.gov/data/data-we- collect/teds-treatment-episode-data-set/datafiles
ACKNOWLEDGEMENTS
Declared none.


